Reid attempts to end cancer drug prescription variation
The Health Secretary has launched a new initiative to end regional differences in the prescribing of drugs to cancer patients.
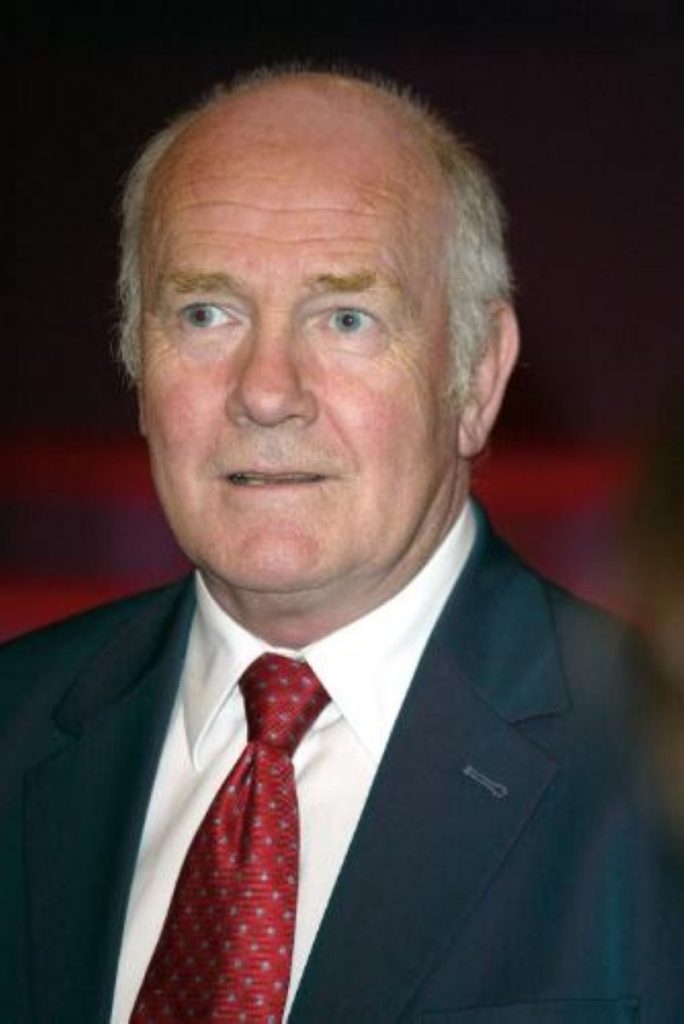
Publishing a report by the National Cancer Director, Professor Mike Richards, Dr John Reid admitted the report showed “unacceptably high variations across the country in the uptake of cancer drugs approved by NICE [the National Institute for Clinical Excellence]”.
The report emphasises that funding issues are not to blame for the variation, and instead highlights constraints of service capacity and differences in clinical practise.
Dr Reid said: “We have seen major progress made in fighting cancer, with a ten per cent fall in premature death rates since 1996. But I recognise there is more to do.


“Better information about regional variations in practice is a key lever in reducing these differences. If we can tell doctors in one area that they seem to be using a particular drug much less than colleagues elsewhere, that provides a trigger for them to reassess their own practices.”
He said electronic hospital prescribing would be introduced in 2006 rather than 2008-10 to identify areas where few drugs were being prescribed.
And as a stopgap measure, commercial firm IMS had agreed to share with the NHS its data on what drugs were being prescribed where.
Other measures included a review of how NICE gives guidance to NHS staff on which drugs and treatments they should use, full costing of NICE recommendations, and closer collaboration between NICE and the NHS.
“I am determined to ensure patients across the country have access to drugs which can help them,” Dr Reid said.
Explaining the recommendations of his report, Professor Richards said that a lack of space and trained doctors are the main reasons for variations in the prescribing of cancer drugs, along with the personal preferences of individual doctors.
He recommended that NICE make sure its evaluations included a report on the resources needed to deliver the drug. The Department of Health should develop a planning capacity model for chemotherapy he said.
Information was the key to changing clinical practice, he said. A ‘robust’ mechanism should therefore be put in place to provide feedback to doctors on their prescribing habits.
“Experience in other aspects of healthcare suggests that this would have a major influence on standardisation of usage across the country. To make this possible, it is essential for electronic prescribing systems to be installed in every hospital providing a chemotherapy service.” Professor Richards concluded.